FDA Restricts Use of 2 Monoclonal Antibody Treatments
The U.S. Food and Drug Administration (FDA) announced Jan. 24 it is restricting the use of two monoclonal antibody treatments for COVID-19, saying data show such treatments are “highly unlikely” to be active against the Omicron variant, currently the dominant strain in the country.
Monoclonal antibodies are laboratory-created proteins that mimic natural antibodies the body produces to fight off harmful pathogens, such as the CCP (Chinese Communist Party) virus, also known as the novel coronavirus.
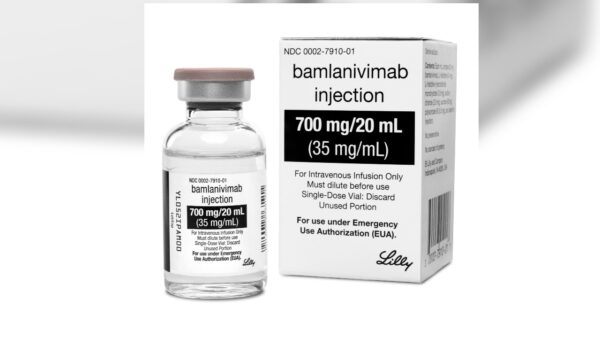
The agency revised its emergency authorization for the two COVID-19 treatments that come from Regeneron and Eli Lilly. Their use is now limited to when the COVID-19 patient is “likely to have been infected with or exposed to a variant that is susceptible to these treatments.”
“Because data show these treatments are highly unlikely to be active against the Omicron variant, which is circulating at a very high frequency throughout the United States, these treatments are not authorized for use in any U.S. states, territories, and jurisdictions at this time,” the FDA stated. “In the future, if patients in certain geographic regions are likely to be infected or exposed to a variant that is susceptible to these treatments, then use of these treatments may be authorized in these regions.”
The Omicron variant, which started spreading in the United States in late November 2021, is estimated to account for more than 99 percent of cases in the country as of Jan. 15, according to data from the Centers for Disease Control and Prevention (CDC).
Rationale
The move to revise the emergency authorization “avoids exposing patients to side effects, such as injection site reactions or allergic reactions, which can be potentially serious, from specific treatment agents that are not expected to provide benefit to patients who have been infected with or exposed to the Omicron variant,” the FDA stated.
The move was recently recommended by the COVID-19 Treatment Guidelines Panel, part of the National Institutes of Health (NIH) on Dec. 23, 2021. At the time, the panel said the Omicron variant “is predicted to have markedly reduced susceptibility” to several COVID-19 monoclonal antibodies, “especially bamlanivimab plus etesevimab and casirivimab plus imdevimab.” Eli Lilly’s monoclonal antibody treatments offers bamlanivimab and etesevimab, and Regeneron offers casirivimab and imdevimab.
The panel added that GlakoSmithKline’s (GSK’s) and Vir Biotech’s antibody treatment, sotrovimab, “appears to retain activity against the Omicron variant.”
The U.S. Department of Health and Human Services (HHS) on Dec. 23, 2021, temporarily halted distribution of Regeneron’s and Eli Lilly’s antibody therapies, leaving sotrovimab as the only available treatment at the time.
Distribution was resumed after complaints from governors, including Florida Gov. Ron DeSantis, who asserted the two monoclonal antibody treatments continued to help some COVID-19 patients. At the time, Omicron was circulating but the Delta variant was still the dominant variant in the United States.
The federal government has, since early January, shipped enough doses of the two monoclonal antibody treatments to treat more than 300,000 patients.
A Regeneron spokesperson had said the regulator would provide any potential communication on the topic. Lilly had no immediate comment but pointed to its statement from December 2021 saying its newer antibody candidate, bebtelovimab, maintains neutralization activity against all known variants of concern, including Omicron. The company said earlier this month it is “urgently working with the FDA to make bebtelovimab available under an emergency use authorization,” with a decision expected before April.

Both companies previously announced they were developing new antibodies that target the Omicron variant. Regeneron stated in December 2021, “While Regeneron’s currently authorized REGEN-COV antibodies have diminished potency against Omicron, they are active against Delta, which currently is the most prevalent variant in the U.S.”
Other Treatments
The revision in emergency authorization comes days after the FDA on Jan. 21 expanded approval of the antiviral drug remdesivir to treat more COVID-19 patients. Remdesivir was the first government-approved drug for COVID-19 and was previously limited to treat hospitalized patients. It is now authorized for use in adults and children aged 12 and above early in a COVID-19 infection if the patient faces a high risk of ending up in hospital.
The agency said its move was supported by a study run by the drug’s developer, Gilead Sciences, results of which showed that the drug reduced the risk of hospitalization by 87 percent among COVID-19-positive people. The FDA didn’t cite any independent studies.
The FDA in its statement on Jan. 24 pointed to several other therapies that “are expected to work against the Omicron variant,” intended for patients with mild-to-moderate COVID-19 to prevent progression to severe disease. They include sotrovimab, remdesivir, as well as two new antiviral pills from Pfizer and Merck, Paxlovid, and molnupiravir, both of which are in short supply.
GSK and Vir Biotech are boosting production of their sotrovimab to help meet demand in the United States.
Remdesivir has been linked to kidney disease, gastrointestinal symptoms, and other severe side effects, according to some researchers. According to the FDA, some adverse events associated with remdesivir include allergic reaction, generalized seizure, rash. The WHO in late 2020 recommended against the use of remdesivir for COVID-19.
Pfizer’s Paxlovid is not recommended in those with severe kidney disease, according to the FDA. The agency also warns that “caution should be exercised” in giving Paxlovid to people with pre-existing liver diseases.
Meanwhile, some experts have expressed concerns about how Merck’s molnupiravir attacks the CCP virus, saying the pill has the potential to contribute to the development of cancer or cause birth defects in an unborn baby.
According to the FDA, sotrovimab may trigger a range of allergic reactions following infusion. The agency also noted, “It is possible that sotrovimab could interfere with your body’s own ability to fight off a future infection of SARS-CoV-2.
“Similarly, sotrovimab may reduce your body’s immune response to a vaccine for SARSCoV-2. Specific studies have not been conducted to address these possible risks. Talk to your healthcare provider if you have any questions.”
https://www.theepochtimes.com/fda-restricts-use-of-2-monoclonal-antibody-treatments_4233896.html?
Reuters contributed to this report.


No comments:
Post a Comment