Is Natural Immunity More Effective Than the COVID-19 Shot?
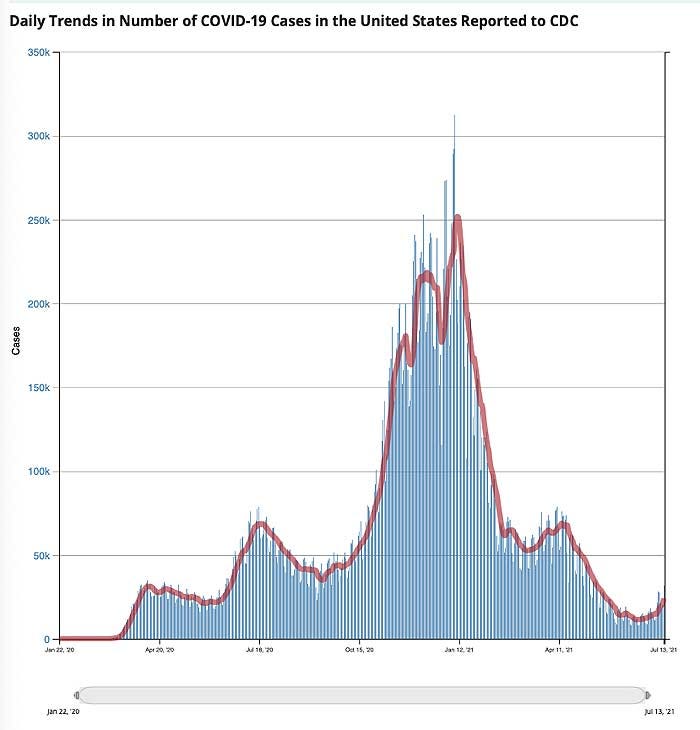
At first glance, this decline appears to be occurring in tandem with the rollout of COVID shots. January 1, 2021, only 0.5% of the U.S. population had received a COVID shot. By mid-April, an estimated 31% had received one or more shots, and as of July 13, 48.3% were fully “vaccinated.”
However, as noted in a July 12, 2021, STAT News article,“cases” had started their downward trend before COVID shots were widely used. “Following patterns from previous pandemics, the precipitous decline in new cases of Covid-19 started well before a meaningful number of people had been vaccinated,” Robert M. Kaplan, Professor Emeritus at the UCLA Fielding School of Public Health, writes. He continues:
“Nearly 50 years ago, medical sociologists John and Sonja McKinlay examined death rates from 10 serious diseases: tuberculosis, scarlet fever, influenzae, pneumonia, diphtheria, whooping cough, measles, smallpox, typhoid, and polio. In each case, the new therapy or vaccine credited with overcoming it was introduced well after the disease was in decline.
More recently, historian Thomas McKeown noted that deaths from bronchitis, pneumonia, and influenza had begun rapidly falling 35 years before the introduction of new medicines that were credited with their conquest. These historical analyses are relevant to the current pandemic.”
‘Case’ Decline Preceded Widespread Implementation of Vaccine
As noted by Kaplan, COVID-19 “cases” peaked in early January 2021. January 8, more than 300,000 new positive test results were recorded on a daily basis. By February 21, that had declined to a daily new case count of 55,000. COVID-19 vaccine injections were granted emergency use authorization at the end of December 2020, but by February 21, only 5.9% of American adults had been fully vaccinated with two doses.
Despite such a low vaccination rate, new “cases” had declined by 82%. Considering health authorities claim we need 70% of Americans vaccinated in order to achieve herd immunity and stop the spread of this virus..
Natural Immunity Explains Decline in Cases
As noted by Kaplan, the most reasonable explanation for declining rates of SARS-CoV-2 appears to be natural immunity from previous infections, which vary considerably from state to state. He goes on to cite a study by the National Institutes of Health, which suggests SARS-CoV-2 prevalence was 4.8 times higher than previously thought, thanks to undiagnosed infection.
In other words, they claim that for every reported positive test result, there were likely nearly five additional people who had the infection but didn’t get a diagnosis. To analyze this data further, Kaplan calculated the natural immunity rate by dividing the new estimated number of people naturally infected by the population of any given state. He writes:
“By mid-February 2021, an estimated 150 million people in the U.S. (30 million times five) may have had been infected with SARS-CoV-2. By April, I estimated the natural immunity rate to be above 55% in 10 states: Arizona, Iowa, Nebraska, North Dakota, Oklahoma, Rhode Island, South Dakota, Tennessee, Utah, and Wisconsin.
At the other end of the continuum, I estimated the natural immunity rate to be below 35% in the District of Columbia, Hawaii, Maine, Maryland, New Hampshire, Oregon, Puerto Rico, Vermont, Virginia, and Washington …
By the end of 2020, new infections were already rapidly declining in nearly all of the 10 states where the majority may have had natural immunity, well before more than a minuscule percentage of Americans were fully vaccinated. In 80% of these states, the day when new cases were at their peak occurred before vaccines were available.
In contrast, the 10 states with lower rates of previous infections were much more likely to experience new upticks in Covid-19 cases in March and April … By the end of May, states with fewer new infections had significantly lower vaccination rates than states with more new infections.”
COVID Shots Cannot Eliminate COVID-19
So, SARS-CoV-2 cases were actually higher in states where natural immunity was low but vaccination rates were high. Meanwhile, in states where natural immunity due to undiagnosed exposure was high, but vaccination rates were low, the daily new caseload was also lower.
This makes sense if natural immunity is highly effective (which, historically it has always been and there’s no reason to suspect SARS-CoV-2 is any different in that regard). It also makes sense if the COVID shots aren’t really offering any significant protection against infection, which we also know is the case.
“The survivability of COVID-19 outside of nursing homes is 99.74%. If you’re under the age of 40, your chance of surviving a bout of COVID-19 is 99.99%.”
Vaccine manufacturers have already admitted these COVID shots will not provide immunity, meaning they will not prevent you from being infected. The idea behind these injections is that if/when you do get infected, you’ll hopefully experience milder symptoms, even though you’re still infectious and can spread the virus to others.
Kaplan ends his analysis by saying that COVID shots are a safer way to achieve herd immunity, and that they are “the best tool available for assuring that the smoldering fire of [COVID-19] is extinguished.”
Vaccine Provides Far Less Protection Than Natural Immunity
While some claim vaccine-induced immunity offers greater protection against SARS-CoV-2 infection than natural immunity, historical and current real-world data simply fail to support this assertion.
As recently reported by Attkisson and David Rosenberg Israeli National News, recent Israeli data show those who have received the COVID jab are 6.72 times more likely to get infected than people who have recovered from natural infection.
Among the 7,700 new COVID cases diagnosed so far during the current wave of infections that began in May 2021, 39% were vaccinated (about 3,000 cases), 1% (72 patients) had recovered from a previous SARS-CoV-2 infection and 60% were neither vaccinated nor previously infected. Israeli National News notes:
“With a total of 835,792 Israelis known to have recovered from the virus, the 72 instances of reinfection amount to 0.0086% of people who were already infected with COVID.
By contrast, Israelis who were vaccinated were 6.72 times more likely to get infected after the shot than after natural infection, with over 3,000 of the 5,193,499, or 0.0578%, of Israelis who were vaccinated getting infected in the latest wave.”
Breakthrough Infections Are on the Rise
Other Israeli data also suggest the limited protection offered by the COVID shot is rapidly eroding. August 1, 2021, director of Israel’s Public Health Services, Dr. Sharon Alroy-Preis, announced half of all COVID-19 infections were among the fully vaccinated. Signs of more serious disease among fully vaccinated are also emerging, she said, particularly in those over the age of 60.
Even worse, August 5, Dr. Kobi Haviv, director of the Herzog Hospital in Jerusalem, appeared on Channel 13 News, reporting that 95% of severely ill COVID-19 patients are fully vaccinated, and that they make up 85% to 90% of COVID-related hospitalizations overall.
Other areas where a clear majority of residents have been vaccinated are also seeing spikes in breakthrough cases. In Gibraltar, which has a 99% COVID jab compliance rate, COVID cases have risen by 2,500% since June 1, 2021.
Natural Immunity Appears Robust and Long-Lasting
An argument we’re starting to hear more of now is that even though natural immunity after recovery from infection appears to be quite good, “we don’t know how long it’ll last.” This is rather disingenuous, seeing how natural immunity is typically lifelong, and studies have shown natural immunity against SARS-CoV-2 is at bare minimum longer lasting than vaccine-induced immunity.
Here’s a sampling of scholarly publications that have investigated natural immunity as it pertains to SARS-CoV-2 infection. There are several more in addition to these:
- Science Immunology October 2020 found that “RBD-targeted antibodies are excellent markers of previous and recent infection, that differential isotype measurements can help distinguish between recent and older infections, and that IgG responses persist over the first few months after infection and are highly correlated with neutralizing antibodies.”
- The BMJ January 2021 concluded that “Of 11, 000 health care workers who had proved evidence of infection during the first wave of the pandemic in the U.K. between March and April 2020, none had symptomatic reinfection in the second wave of the virus between October and November 2020.”
- Science February 2021 reported that “Substantial immune memory is generated after COVID-19, involving all four major types of immune memory [antibodies, memory B cells, memory CD8+ T cells, and memory CD4+ T cells]. About 95% of subjects retained immune memory at ~6 months after infection. Circulating antibody titers were not predictive of T cell memory.Thus, simple serological tests for SARS-CoV-2 antibodies do not reflect the richness and durability of immune memory to SARS-CoV-2.” A 2,800-person study found no symptomatic reinfections over a ~118-day window, and a 1,246-person study observed no symptomatic reinfections over 6 months.
- A February 2021 study posted on the prepublication server medRxiv concluded that “Natural infection appears to elicit strong protection against reinfection with an efficacy ~95% for at least seven months.”
- An April 2021 study posted on medRxiv reported “the overall estimated level of protection from prior SARS-CoV-2 infection for documented infection is 94.8%; hospitalization 94.1%; and severe illness 96·4%. Our results question the need to vaccinate previously-infected individuals.”
- Another April 2021 study posted on the preprint server BioRxiv concluded that “following a typical case of mild COVID-19, SARS-CoV-2-specific CD8+ T cells not only persist but continuously differentiate in a coordinated fashion well into convalescence, into a state characteristic of long-lived, self-renewing memory.”
- A May 2020 report in the journal Immunity confirmed that SARS-CoV-2-specific neutralizing antibodies are detected in COVID-19 convalescent subjects, as well as cellular immune responses. Here, they found that neutralizing antibody titers do correlate with the number of virus-specific T cells.
- A May 2021 Nature article found SARS-CoV-2 infection induces long-lived bone marrow plasma cells, which are a crucial source of protective antibodies. Even after mild infection, anti-SARS-CoV-2 spike protein antibodies were detectable beyond 11 months’ post-infection.
- A May 2021 study in E Clinical Medicine found “antibody detection is possible for almost a year post-natural infection of COVID-19.” According to the authors, “Based on current evidence, we hypothesize that antibodies to both S and N-proteins after natural infection may persist for longer than previously thought, thereby providing evidence of sustainability that may influence post-pandemic planning.”
- Cure-Hub data confirm that while COVID shots can generate higher antibody levels than natural infection, this does not mean vaccine-induced immunity is more protective. Importantly, natural immunity confers much wider protection as your body recognizes all five proteins of the virus and not just one. With the COVID vaccine, your body only recognizes one of these proteins, the spike protein.
- A June 2021 Nature article points out that “Wang et al. show that, between 6 and 12 months after infection, the concentration of neutralizing antibodies remains unchanged. That the acute immune reaction extends even beyond six months is suggested by the authors’ analysis of SARS-CoV-2-specific memory B cells in the blood of the convalescent individuals over the course of the year.These memory B cells continuously enhance the reactivity of their SARS-CoV-2-specific antibodies through a process known as somatic hypermutation. The good news is that the evidence thus far predicts that infection with SARS-CoV-2 induces long-term immunity in most individuals.”
- Another June Nature paper concluded that “In the absence of vaccination antibody reactivity [to the receptor binding domain (RBD) of SARS-CoV-2], neutralizing activity and the number of RBD-specific memory B cells remain relatively stable from 6 to 12 months.” According to the authors, the data suggest “immunity in convalescent individuals will be very long lasting.”
What Makes Natural Immunity Superior?
The reason natural immunity is superior to vaccine-induced immunity is because viruses contain five different proteins. The COVID vaccine induces antibodies against just one of those proteins, the spike protein, and no T cell immunity. When you’re infected with the whole virus, you develop antibodies against all parts of the virus, plus memory T cells.
This also means natural immunity offers better protection against variants, as it recognizes several parts of the virus. If there are significant alternations to the spike protein, as with the Delta variant, vaccine-induced immunity can be evaded. Not so with natural immunity, as the other proteins are still recognized and attacked.
References:
- COVID.CDC.gov, COVID Cases in the US Reported to the CDC, Viewed July 15, 2021
- Bloomberg COVID Vaccine Tracker, see US Vaccinations vs Cases graph, top portion
- Mayo Clinic COVID Vaccine Tracker
- STAT News July 12, 2021
- Health and Society 1977; 55(3): 405-428
- Population Studies, A Journal of Demography 1975; 29(3): 391-422
- NIH.gov June 22, 2021
- Annals of Internal Medicine September 2, 2020 DOI: 10.7326/M20-5352
- Greek Reporter June 27, 2020
- WFAE.org July 2, 2020
- medRxiv June 1, 2021
- U.S. CDC, COVID-19 Vaccination FAQs April 30, 2021
- Medium February 15, 2021
- Sharylattkisson.com August 8, 2021
- David Rosenberg 7 July 13, 2021
- Bloomberg August 1, 2021 (Archived)
- American Faith August 8, 2021
- Big League Politics August 4, 2021
- CDC MMWR July 30, 2021; 70
- CNBC July 30, 2021
- NBC News August 7, 2021
- Sharylattkisson.com August 6, 2021
- NBC Chicago July 28, 2021
- Reddit COVID-19 and Immunity
- Science Immunology October 8, 2020; 5(52): eabe0367
- BMJ 2021;372:n99
- Science February 5, 2021; 371(6529): eabf4063
- medrxiv February 8, 2021 DOI: 10.1101/2021.01.15.21249731
- medRxiv April 24, 2021 (PDF)
- BioRxiv April 29, 2021 DOI: 10.1101/2021.04.28.441880
- Immunity June 16, 2020; 52(6): 971-977.E3
- Nature 2021; 595: 421-425
- E Clinical Medicine 2021; 36: 100902 (PDF)
- Cure-hub June 11, 2021
- Nature June 14, 2021
- The Hill August 5, 2021
- Vaccines 2021; 9(7): 693

No comments:
Post a Comment